From 1 piece to mass production, our one-stop custom services ensure a worry-free experience for you.
Help Center
Views: 222 Author: Rebecca Publish Time: 2026-01-27 Origin: Site
Content Menu
● What is additive manufacturing in the medical industry?
● What is traditional manufacturing in the medical industry?
● Main additive processes for medical devices
>> Fused Deposition Modeling (FDM)
>> Selective Laser Sintering (SLS)
>> Direct Metal Laser Sintering (DMLS)
● Main traditional processes for medical devices
>> Injection molding and medical‑grade tooling
>> Sheet metal fabrication and stamping
● Comparison table: additive vs traditional manufacturing in medical
● When to choose additive vs traditional in the medical industry
● Hybrid manufacturing: combining additive with CNC machining and molding
● Practical decision framework for medical device teams
● Real‑world examples of additive vs traditional in medical manufacturing
● How OEM buyers can work with a manufacturing partner like U-NEED
● Action call for your next medical project
● Frequently asked questions (FAQ)
>> 1. Is additive manufacturing approved for medical implants?
>> 2. When does injection molding beat 3D printing for medical parts?
>> 3. Can I combine 3D printing and CNC machining on the same medical part?
>> 4. Which materials are most common for 3D‑printed medical components?
>> 5. How do I decide if a medical prototype should be 3D printed or machined?
Choosing between additive manufacturing and traditional manufacturing for medical devices directly affects regulatory approval, patient safety, and total product cost. For overseas brands, wholesalers, and OEM producers working with suppliers like U-NEED in China, understanding when to use each process – or a hybrid of both – is essential to build a robust, scalable medical product supply chain.

Additive manufacturing, often called 3D printing, builds parts layer by layer directly from a digital model, which allows extremely complex geometries and patient‑specific designs. In the medical industry, it is widely used for surgical guides, anatomical models, custom prosthetics, dental devices, and increasingly, functional end‑use components and implants.
Key benefits of additive manufacturing for medical:
- Mass customization for patient‑specific implants, braces, and surgical guides.
- Rapid prototyping to iterate designs in days instead of weeks.
- Complex internal structures to optimize weight, stiffness, and bone integration.
- Localized production close to hospitals or regional warehouses, reducing inventory and lead times.
Common limitations of additive manufacturing:
- Surface finish often requires post‑processing to meet clinical and aesthetic standards.
- Build size and throughput constraints can make very large or very high‑volume parts less economical.
- Validation can be more complex for new materials and novel workflows.
Traditional manufacturing uses established subtractive and forming processes such as CNC machining, injection molding, tooling, and sheet metal fabrication. These processes dominate high‑volume production of surgical instruments, metal implants, disposable plastic components, housings, and structural frames for medical equipment.
Core advantages of traditional processes:
- Tight tolerances and excellent surface finish on critical features using CNC machining.
- Very low piece‑part cost in large volumes with injection molding and progressive stamping.
- Stable, well‑understood materials with long histories in medical devices.
- High repeatability and process control for long production runs and global supply programs.
Typical limitations of traditional methods:
- High up‑front tooling costs and longer setup times, especially for molding and complex stamping dies.
- Less flexible for rapid design changes once tooling is built.
- More material waste for complex machined components.
MJF uses a fusing agent and infrared energy to create detailed polymer parts with strong mechanical properties.
Strengths:
- High precision and fine detail for complex geometries.
- Faster than many other additive methods, suitable for rapid prototyping and bridge production.
- Good material flexibility, including nylon and TPU for functional components and flexible devices.
Considerations:
- Raw surface finish can be slightly grainy and usually needs bead blasting or coating for patient‑facing surfaces.
- Best suited for small to medium‑sized parts within the build volume of the printer.
Typical medical applications: custom prosthetics, orthotic shells, ergonomic instrument handles, and surgical guides.
FDM extrudes thermoplastic filament layer by layer and is widely used for early prototypes and low‑risk fixtures.
Strengths:
- Cost‑effective for initial models and low‑volume parts.
- Wide material range, including ABS, PLA, and higher‑performance engineering materials.
Considerations:
- Visible layer lines; parts may require sanding, coating, or machining if used in clinical environments.
- Lower mechanical properties than advanced additive processes, which may limit use in high‑load applications.
Typical medical applications: design verification models, jigs and fixtures, non‑sterile handling tools, and basic anatomical models for training.
SLS uses a laser to sinter powdered polymer into solid parts, eliminating the need for support structures.
Strengths:
- Support‑free building enables very complex shapes, including internal channels and living hinges.
- Robust mechanical properties suitable for functional prototypes and some end‑use parts.
Considerations:
- Powder handling and post‑processing require controlled environments and skilled operators.
- Surface finish can be matte and porous; sealing or coating may be needed for certain applications.
Typical medical applications: functional prototypes, housings, patient‑specific guides, and lightweight orthotic components.
DMLS and similar metal powder bed fusion processes create dense metal parts with excellent mechanical performance.
Strengths:
- High precision and strength, suitable for load‑bearing implants and complex surgical tools.
- Compatible with biocompatible metals such as titanium, stainless steel, and cobalt‑chrome.
Considerations:
- Higher part cost compared with polymer additive processes and significant post‑processing requirements.
- Validation and quality control must be rigorous to satisfy implant standards.
Typical medical applications: spinal cages, dental implants, patient‑specific joint components, and complex surgical instruments.
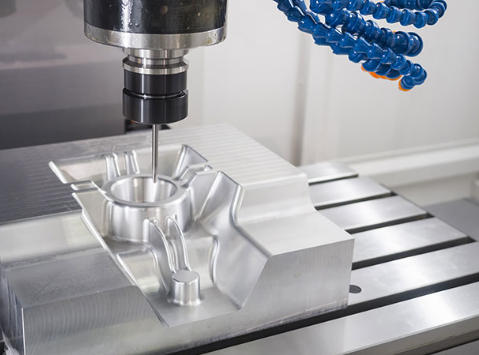
CNC machining removes material from metal or plastic stock to achieve precise shapes and tight tolerances.
Strengths:
- Exceptional precision and accuracy with fine surface finishes.
- Works with titanium, stainless steel, aluminum, PEEK, and many engineering plastics.
Considerations:
- Higher setup time and cost per program; less efficient for frequent design changes.
- Material waste can be high, especially for deep pockets and complex 3D surfaces.
Typical medical applications: surgical instruments, orthopedic implants, high‑precision connectors, and valve components.
Injection molding injects molten plastic into a metal mold, making it ideal for high‑volume disposable or semi‑disposable components.
Strengths:
- Very low unit cost for large volumes once molds are built.
- High consistency and repeatability across large production runs.
- Broad range of medical‑grade materials, including polypropylene, ABS, polycarbonate, and silicones.
Considerations:
- Tooling typically demands significant initial investment and several weeks to complete.
- Design changes after tool cutting are costly and time‑consuming.
Typical medical applications: syringe bodies, connectors, diagnostic device housings, pump components, and soft silicone parts.
Sheet metal processes cut, bend, and form metal sheets, while stamping uses dies to press features at high speed.
Strengths:
- Efficient for enclosures, chassis, and mounting brackets used in diagnostic equipment and hospital devices.
- Progressive die stamping achieves very low cycle times and consistent output for metal clips, springs, and contacts.
Considerations:
- Custom dies and tools can be expensive for complex geometries.
- Limited suitability for highly 3D organic shapes.
Typical medical applications: frames for imaging equipment, control panels, shielding and covers, and stamped components within devices.
| Dimension | Additive manufacturing (AM) | Traditional manufacturing |
|---|---|---|
| Design flexibility | Excellent for complex, lattice, and patient‑specific geometries. | Best for prismatic, symmetric, and standardized designs. |
| Customization | High, ideal for one‑off or small‑batch personalized devices. | Limited; customization usually requires custom tooling or fixtures. |
| Volume economics | Most cost‑effective at low to medium volumes. | Most cost‑effective at medium to very high volumes. |
| Lead time for first parts | Very short; parts in days with no hard tooling. | Longer due to tooling, programming, and setup. |
| Surface finish | Often requires post‑processing for clinical use. | Excellent finish achievable directly from machining, molding, and polishing. |
| Regulatory familiarity | Newer but rapidly maturing; requires clear process validation. | Well‑established process histories and standards. |
| Material options | Advanced polymers and metals, including some biocompatible grades. | Broad portfolio of certified medical‑grade metals and plastics. |
| Typical medical use cases | Surgical guides, anatomical models, custom implants and prosthetics. | Surgical tools, mass‑produced disposables, housings, and high‑volume implants. |
You can decide between additive and traditional methods by mapping your part against a few critical dimensions: design complexity, required quantity, material and performance targets, and risk level. In many projects, the optimal solution is not “either‑or” but a staged or hybrid approach.
Additive manufacturing is usually the better choice when:
1. You need patient‑specific geometry, such as custom implants, prosthetics, or surgical guides.
2. The design is still evolving and you want fast iteration with minimal tooling cost.
3. Internal channels, lattice structures, or highly organic shapes are essential for function.
Traditional manufacturing is usually the better choice when:
1. You have validated the design and need stable, high‑volume production.
2. Tight tolerances and surface quality are critical and based on well‑known processes.
3. The part geometry is relatively simple or standardized, making molding, machining, or stamping efficient.
Many leading medical manufacturers increasingly adopt hybrid manufacturing, combining additive and traditional processes in one workflow. Integrating 3D printing with CNC machining can significantly reduce total production costs and shorten processing cycles for complex parts, compared with using only conventional methods.
How hybrid workflows improve medical parts:
- Use additive methods to create near‑net‑shape blanks or internal structures, then refine critical surfaces and interfaces via CNC machining.
- Print complex polymer components during development, then transfer high‑volume SKUs into injection molding once designs and volumes stabilize.
- Replace multi‑part assemblies with a single 3D‑printed structure, machining only tightly toleranced features such as sealing surfaces and joint interfaces.
This kind of combined strategy allows medical OEMs to balance speed, cost, and compliance throughout the product life cycle.
To choose the right process for a new medical component, you can follow a simple, repeatable framework.
1. Define clinical and risk level.
Higher‑risk implants and life‑critical tools usually benefit from well‑documented materials and processes, often favoring machining, molding, or hybrid approaches.
2. Classify volume and product life cycle.
Early‑stage devices and low‑volume customized solutions align well with additive methods, while stable, long‑life, high‑volume products typically favor traditional production.
3. Assess geometry and complexity.
If the geometry includes complex lattices or organic shapes that are hard to mill or mold, additive or hybrid workflows are likely more effective.
4. Evaluate material and mechanical requirements.
Confirm whether the needed biocompatible metals or polymers are available and validated for your chosen process.
5. Model cost and lead time over the full life cycle.
Include tooling costs, design change likelihood, validation effort, and service‑life updates rather than only comparing unit prices.
This framework makes decisions about additive and traditional processes traceable and defendable during regulatory reviews and supplier audits.
Example 1 – Custom surgical guides
Hospitals often use CT‑based anatomical data to generate 3D‑printed surgical guides that match the patient's bone structure, enabling more accurate cuts and shorter operation times. These guides are typically produced via polymer additive processes because each part is unique and required in very low volume.
Example 2 – High‑volume disposable components
Disposable syringe bodies and diagnostic cassette housings usually run in very high quantities per year, making injection molding with hardened steel tooling the most economical and repeatable solution. Additive methods are typically used at the prototype stage or for design verification models.
Example 3 – Complex metal implants
For intricate spinal cages or porous bone‑contact surfaces, metal powder bed fusion allows integrated lattice structures that promote bone in‑growth and reduce weight, which are difficult to machine conventionally. Critical contact areas may still be CNC‑machined afterward to meet tolerance and finish requirements.
For overseas brands and wholesalers, the biggest challenge is often not the technology itself but integrating it into a reliable, compliant supply chain. Working with an experienced Chinese OEM that offers CNC machining, plastic and silicone molding, metal stamping, and access to additive services allows buyers to test different production routes without changing suppliers.
When evaluating a partner for medical projects, look for:
- Proven experience with tight tolerances and medical‑grade materials in machining, molding, and stamping.
- Ability to support prototype‑to‑production transitions, including additive prototyping and traditional scale‑up.
- Quality systems aligned with medical expectations, including documented process control, traceability, and robust inspection.
- Transparent communication on risk, validation requirements, and design‑for‑manufacturability feedback.
A partner like U-NEED can help you compare processes for each component, suggest hybrid paths, and then lock in the most efficient method once your design and demand are stable.
If you are preparing a new medical device or component and still comparing additive and traditional manufacturing options, this is the right time to get engineering feedback from a production‑ready supplier. Send your CAD files, target quantities, and basic regulatory requirements to U-NEED so our team can review your design, propose additive, traditional, or hybrid production routes, and give you clear lead time and cost estimates tailored to your medical application.
Contact us to get more information!

Regulators have already cleared many 3D‑printed implants and patient‑specific devices, especially in orthopedics and dental, when they use validated materials and processes. However, each device still needs its own risk assessment, verification, and regulatory submission.
Injection molding becomes more economical when volumes rise and designs are stable because tooling cost is spread across large production runs. Additive methods are usually better for early prototypes, small batches, or highly customized parts where no hard tooling is justified.
Yes, many manufacturers now use additive methods to create near‑net shapes and CNC machining for critical surfaces and interfaces, especially for complex metal implants and housings. This hybrid approach can reduce cost and lead time while still achieving very tight tolerances where needed.
Common materials include nylon and TPU for polymer parts, and titanium, stainless steel, and cobalt‑chrome for metal implants and tools. New bio‑compatible materials and bio‑inks are also emerging for future tissue and organ‑related applications.
If you need one‑off or low‑volume parts with complex geometry and quick turnaround, 3D printing is usually the first choice. If you require very tight tolerances, specific surface finishes, or closer representation of final machined metal parts, CNC machining may be more appropriate even for prototypes.
1. https://uptivemfg.com/additive-vs-traditional-manufacturing-in-the-medical-industry-choosing-the-right-process/
2. https://pmc.ncbi.nlm.nih.gov/articles/PMC10912264/
3. https://aipprecision.com/medical-machined-components-why-cnc-3d-printing-outperforms-traditional-methods/
4. https://www.bioaccessla.com/br/blog/comparing-surgical-instruments-manufacturing-traditional-vs-additive
5. https://amfg.ai/2025/02/05/additive-manufacturing-forecast-2025-technology-and-applications/
content is empty!